BNA Annual General Meeting 2025
1st April 2025
28th Apr 2020
Jordan Truong, undergraduate student in Neuroscience, University of Southampton
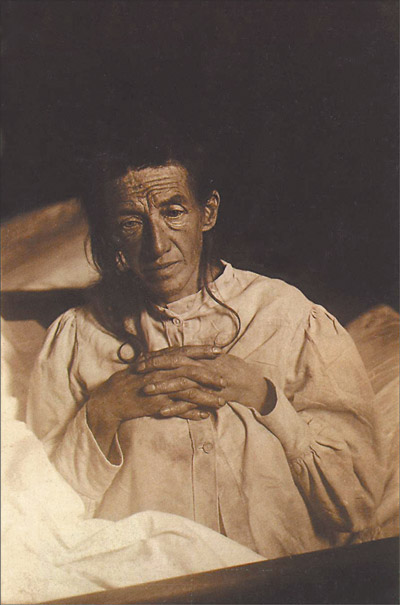 Over 100 years ago the German psychiatrist Alois Alzheimer published his post-mortem neuropathological observations in former patient Auguste Deter, who had exhibited a complete degeneration of the psyche in the years before her death, and whose brain showed the now-classic hallmarks of senile plaques and neurofibrillary tangles in the disease that now bears his name[1].
Over 100 years ago the German psychiatrist Alois Alzheimer published his post-mortem neuropathological observations in former patient Auguste Deter, who had exhibited a complete degeneration of the psyche in the years before her death, and whose brain showed the now-classic hallmarks of senile plaques and neurofibrillary tangles in the disease that now bears his name[1].
100 years later, Alzheimer’s disease (AD) is an ever-growing public health problem with up to 1 million cases expected in the UK by 2025, and the clinical effects of cognitive decline and dementia (of which AD is the most common cause) remain as devastating as ever.
Much of the research into the pathogenesis and treatments for AD has focused on the ‘Amyloid Cascade Hypothesis’ that places the neuro-pathological proteins of Amyloid-beta and tau[2] as the primary disease effectors. Despite this, with the U.S. NIH spending $1.9 billion on research in 2018 alone, our understanding of AD has not progressed much further; the failure rate of AD drug clinical trials currently stands at 99%.
As a result, scientists have begun to think ‘outside the box’ to consider the multifaceted origins of AD, and the multiple peripheral health conditions (such as diabetes and gum disease) that could increase the risk of patients developing the condition. Significant research has also focused on the causes and prevention of neuroinflammation, another clinical observation in dementia-afflicted brains.
 From epidemiological studies[3] in older populations, it was observed that people who had lost teeth as a result of gum disease earlier in life were more likely to develop AD. This was theorised to be from molecules called cytokines being released into the general blood circulation as a result of periodontal inflammation. Cytokines could then migrate to the brain and activate the resident macrophages (microglia) into an immune-inflammatory response[4] that exacerbates the neuropathology of AD, leading to brain atrophy and dementia.
From epidemiological studies[3] in older populations, it was observed that people who had lost teeth as a result of gum disease earlier in life were more likely to develop AD. This was theorised to be from molecules called cytokines being released into the general blood circulation as a result of periodontal inflammation. Cytokines could then migrate to the brain and activate the resident macrophages (microglia) into an immune-inflammatory response[4] that exacerbates the neuropathology of AD, leading to brain atrophy and dementia.
A landmark study[5] into the role of periodontitis in AD additionally focused on the oral bacteria Porphyromonas gingivalis, and how it acts in conjunction with neuroinflammation to cause AD. Oral infection in mice with this ‘keystone pathogen’ directly led to the formation of senile plaques and neurodegeneration. Furthermore, a small-molecule inhibitor targeting the pathogenic enzymes in Pg reduced the bacterial load, blocked plaque production, reduced neuroinflammation, and rescued hippocampal neurons.
These results have significant implications for gum disease as an environmentally-modifiable risk factor for AD; further research will focus on how exactly transient bacteraemia of Pg occurs from gums to brain to exert neurotoxicity. Early interventions[6] aimed at preventing AD through periodontal treatment and oral hygiene in the general population may thus prove to be extremely effective in reducing the future incidence of dementia.
References:
1. Strange. P.G. (1992) ‘Brain Biochemistry and Brain Disorders’ // Oxford University Press
2. Sorrentino. G. & Bonavita. V. (2007) ‘Neurodegeneration and Alzheimer’s disease: the lesson from tauopathies.’ // Neurol. Sci. 28: 63-71
3. Ide. M, et. al. (2016) ‘Periodontitis and Cognitive Decline in Alzheimer’s disease.’ // PLOS One. 11(3)
4. Teixeira. F.B, et. al. (2017) ‘Periodontitis and Alzheimer’s disease: A possible comorbidity between oral chronic inflammatory condition and neuroinflammation.’ // Front. Aging Neurosci. 9: 327
5. Dominy. S, et. al. (2019) ‘Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors.’ // Sci. Adv. 5: eaau3333
6. Singhrao. S.K, et. al. (2017) ‘Can better management of periodontal disease delay the onset and progression of Alzheimer’s disease?’ // J. Alzheimer’s Dis. 58(2): 337-348